– The supply of care services is slowing in response to the increase in the elderly population, leading to a deterioration in all indicators, including public care, senior housing, and nursing care costs.
Expanding senior housing supply can also reduce social care costs… Urgent practical measures are needed to address the care gap.
As the elderly population in Korea rapidly increases, exceeding 10 million, it has been analyzed that the supply of elderly care is not keeping up with demand, resulting in a growing 'care blind spot' every year.
Caredoc (CEO Jae-byung Park), a total senior care company, announced on the 16th that it has released the "2025 Elderly Care Gap Index," a report analyzing the current state of senior care based on public data statistics. This is the second report released since 2023, and it draws attention by revealing that the overall level of the elder care gap has worsened over the past three years.
As a leading player in the domestic senior care market, Caredoc developed the Elderly Care Gap Index to raise awareness of the reality of senior care and encourage effective policymaking and constructive growth in the care industry. Using 2008, the year long-term care insurance was first introduced, as the baseline (100), the index quantifies the level of the care gap annually, allowing for intuitive understanding of changing trends.
Notably, the new report further refines its analysis, using data from 2024, the most recent available, to provide a detailed look at the changing landscape of care. Tailored to the structure of Korea's elderly care system, the report analyzed three key indicators: the Long-Term Care Gap Index, the Senior Housing Gap Index, and the Nursing Care Price Index, and derived the final index based on these analyses.
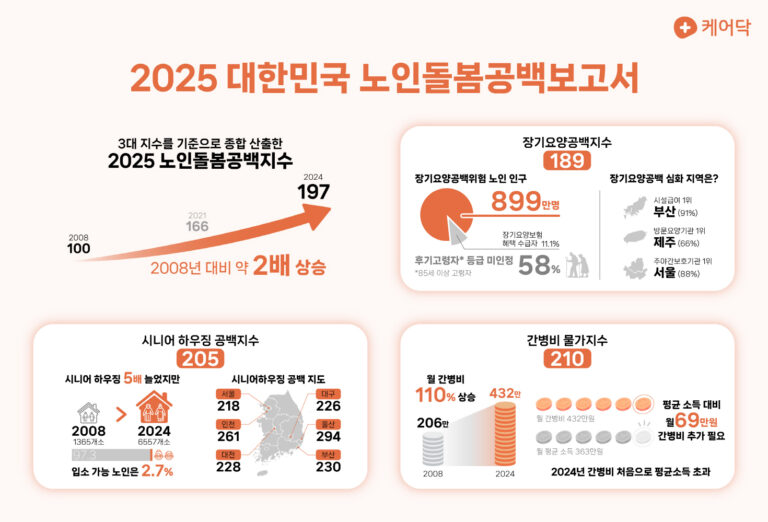
The 2025 Elderly Care Gap Index, which assesses the overall current status, was calculated at 197. This is approximately double the 2008 figure and a 31-point increase compared to 2021 (166). Caredoc CEO Park Jae-byeong explained, "While the overall supply of care services has increased slightly, the care gap is growing." He added, "The main reason for the index increase is that the speed of supply and accessibility across services are not keeping pace with the growth in the elderly population."
Detailed indicators also worsened across the board. First, the Long-Term Care Gap Index, which compiles information on long-term care insurance benefits, recorded 189. By 2025, approximately 8.99 million elderly people, or 89% of the total, are expected to be at risk of a long-term care gap. While the number of beneficiaries has increased fivefold since 2008, to approximately 1.13 million, the overall elderly population is growing at a faster rate, widening the gap. In particular, elderly people aged 85 and older are analyzed as the age group with the highest demand for care and the greatest vulnerability to long-term care gaps.
The risk of long-term care gaps varied by region. Because more than 50% of facilities and institutions covered by long-term care insurance are located in the metropolitan area, regions outside the metropolitan area were at a relatively higher risk of gaps. The gaps varied somewhat by type, with Busan recording the highest gap rate for facility-based care providers (91%) and Jeju Island recording the highest gap rate for home-based care providers (66%). However, due to a decline in the number of day and night care facilities in the metropolitan area, Seoul (88%) actually had the highest gap rate.
The second indicator, the Senior Housing Gap Index, was 205. This index analyzes the supply of "senior housing," which provides care and housing for the elderly, and serves as a measure of the stability of senior housing welfare. While the number of related facilities will increase by about fivefold from 2008 to 6,557 in 2024, the available occupancy will only be about 270,000, or 2.7% of the total elderly population. This means that more than 97% will have no choice but to wait for admission or receive home care. Furthermore, regional senior housing gaps were highest in Ulsan, the top city, as well as major metropolitan cities and Gyeonggi Province. This suggests that access to senior housing services is lower in densely populated areas.
The final sub-index, the Care Cost Price Index, represents the burden of care costs per elderly person. This index reached 210, more than doubling since 2008, revealing a growing burden relative to income. This is also due to the increasing number of young caregivers who are struggling financially as they care for their families instead of working. In fact, the monthly cost of hiring a caregiver in 2025 is projected to be approximately 4.32 million won, an additional 690,000 won above the average income of 3.63 million won. These costs are further exacerbated when elderly people are hospitalized.
The report highlighted the need for a senior housing model as an alternative to alleviating this social care burden. Senior housing, which combines housing and care, is a system that allows for integrated management of housing costs, caregiver skills, food, and supplies. These facilities can prevent inefficient spending and provide high-quality, professional care 24/7, while reducing care costs per senior by up to 40%.
Professor Kim Kyung-min of the Department of Urban Planning at Seoul National University's Graduate School of Environmental Studies said about the Elderly Care Gap Index report, "It is an important indicator that clearly shows in numbers the gap in the long-term care system in a super-aging society and the resulting delay in the supply of senior housing." He added, "In particular, when looking at it from the perspective of housing and welfare infrastructure, which are the core of urban planning, I believe it strongly demonstrates the need for a new housing model supply and care policy suitable for an aging society."
Rep. Eom Tae-young of the National Assembly’s Land, Infrastructure and Transport Committee said, “I think it is meaningful that the private sector has systematically analyzed the reality of the care gap and presented it as an indicator,” and “In particular, since this data serves as a basis for objectively examining the role of care and housing infrastructure, I expect it will also be helpful in establishing future senior housing supply policies and stable models for elderly care.”
Caredoc anticipates that the private sector will play an increasingly important role in preventing the continued worsening of the care gap amid the growing elderly population. It anticipates that private care can contribute to alleviating the care gap by supplementing blind spots in public care while also providing a stable supply of high-quality care. Caredoc is particularly committed to expanding its role as an integrated senior care platform, recognizing the importance of providing more affordable care across the entire senior life cycle, thereby reducing both the social and personal burden.
Caredoc CEO Jae-Byeong Park said, “As elderly care is emerging as a major social issue due to the intertwining of changes in the domestic population structure and system limitations, it is absolutely necessary to take practical measures to resolve the care gap.” He added, “As a leading care platform in the private care sector, Caredoc will continue to take the lead in suggesting policy and industrial directions for establishing a care system based on field data.”
Caredoc's '2025 Elderly Care Gap Index' is available on Caredoc's official blog.
You must be logged in to post a comment.